Most people infected with the COVID-19 virus will have mild to moderate respiratory symptoms and recover without requiring special treatment or hospitalization. Some will have no symptoms at all.
According to the CDC, currently having cancer increases your risk of having serious complications if you do become infected with COVID-19. At this time, it’s not known if having a history of cancer increases your risk of serious complications.
This higher risk for serious complications from COVID-19 for people currently diagnosed with cancer likely is because having cancer puts a strain on the body and also because certain treatments can cause people to become immunocompromised (have a weakened immune system) or have lung problems.
The following breast cancer treatments can weaken the immune system:
- all standard chemotherapy drugs, such as Taxol (chemical name: paclitaxel), Taxotere (chemical name: docetaxel), Cytoxan (chemical name: cyclophosphamide), and carboplatin
- certain targeted therapies, such as Ibrance (chemical name: palbociclib), Kisqali (chemical name: ribociclib), Verzenio (chemical name: abemaciclib), and Piqray (chemical name: alpelisib)
Typically, the immune system recovers within a couple of months after you stop receiving chemotherapy or targeted therapy. But your immune system’s recovery time can vary and depends on several factors. If you received those treatments in the past, it’s not clear if you are at higher risk for serious complications from COVID-19. If you’re receiving ongoing treatment with these medicines for metastatic breast cancer, it’s likely that your immune system is weakened.
Some chemotherapy medicines and targeted therapies can also cause lung problems, which could put people at higher risk for serious COVID-19 complications. Rare but severe lung inflammation has been linked to Ibrance, Kisqali, Verzenio, and the immunotherapy drug Tecentriq (chemical name: atezolizumab).
People with metastatic breast cancer in the lungs also can have lung problems that may get worse if they develop COVID-19.
Some people with breast cancer may have other risk factors for developing serious complications from COVID-19. For example, you are at greater risk if you:
- are age 65 or older; though the risk for serious complications increases with age, so people in their 50s are at higher risk than people in their 40s and people in their 60s and 70s are at higher risk than people in their 50s; the greatest risk for serious complications is among people age 85 and older
- have chronic obstructive pulmonary disease (COPD)
- have a serious heart condition
- have type 2 diabetes, chronic kidney disease, or sickle cell disease
- are obese
- smoke
Research on COVID-19 and cancer is very limited, so it’s not clear how COVID-19 may affect people diagnosed with cancer. It’s also not clear how different types of cancer may affect COVID-19 outcomes.
Research on COVID-19 and cancer is very limited, so it’s not clear how COVID-19 may affect people diagnosed with cancer. It’s also not clear how different types of cancer may affect COVID-19 outcomes.
To provide more information, researchers at Vanderbilt University have launched a project called the COVID-19 and Cancer Consortium (CCC19) to track outcomes of adults diagnosed with cancer around the world who have been infected with COVID-19. More than 100 cancer centers and other organizations are participating.
The first report from this project was published in the Lancet on May 28, 2020, and included information on 928 people diagnosed with cancer in Spain, Canada, and the United States who also were diagnosed with COVID-19. Breast cancer was the most common cancer in the group, affecting about 20% of the people. Half the people were older than 66, and 30% were older than 75.
About 13% of the people in the study died, which is about twice the death rate for all people with COVID-19. A higher risk of dying for people with both cancer and COVID-19 was linked to the same risk factors for people without cancer who get COVID-19, including:
- being older
- having a serious underlying health condition, such as diabetes, kidney disease, or heart problems
- being a man
Thanks to breastcancer.org
The COVID-19 pandemic has affected just about every aspect of life, including screening, diagnosis, treatment, and follow-up care for breast cancer. People who’ve been diagnosed with breast cancer and people who are at high risk for breast cancer have found themselves in a uniquely difficult and sometimes frightening position since the coronavirus crisis began. Many of you are wondering if it’s safe to go to certain medical appointments or if you should postpone treatments or screening. Others have had their treatments delayed or changed.
In this Special Report from Breastcancer.org, we have gathered the most important information you need to know about the impact the coronavirus has had on breast cancer care, including why currently being treated for breast cancer can raise the risk of serious COVID-19 complications, what healthcare facilities are doing to minimize your exposure to the virus when seeking medical care, and how to get the best care possible even if your treatment plan changes.
In March, the Centers for Disease Control and Prevention (CDC), the Centers for Medicare and Medicaid Services (CMS), and local and state governments recommended that healthcare systems delay elective care, meaning surgeries, screenings, and other treatments that are not considered urgent or emergencies. Hospitals began canceling some surgeries and limiting other services to protect people from being exposed to COVID-19 and to save resources such as hospital beds, personal protective equipment (PPE), blood supply, and staff time so they could be used to care for seriously ill patients with COVID-19.
Time will tell whether we made the right decisions in order to try to protect our patients from the virus and take care of the breast cancer,” said Jill Dietz, M.D., FACS, co-founder of the COVID-19 Pandemic Breast Cancer Consortium, president of the American Society of Breast Surgeons, and associate professor of surgery at Case Western Reserve University School of Medicine in Cleveland, Ohio. “Having a diagnosis of breast cancer at any time is very scary, and now it’s especially difficult. I feel so bad for the patients going through breast cancer treatment during the pandemic, and I feel bad for the physicians who were told they can’t practice like they normally practice.”
Doctors are looking at each person’s unique situation and diagnosis when deciding how to best move forward with breast cancer treatment during the pandemic. For example, they are looking at whether a person has a higher risk of becoming seriously ill from a COVID-19 infection due to a weakened immune system from treatments such as chemotherapy or targeted therapy, or because of their age or other health problems.
Healthcare facilities have adopted stricter safety practices to reduce the risk of exposing people to COVID-19. At the same time, many cancer treatment plans have been changed so people don’t have to spend as much time at these facilities. Medical appointments are being spread out to avoid close contact between people, more appointments are being done over the phone or online, and hospital stays after surgery have been shortened. In some cases, fewer in-person visits are required to complete chemotherapy or radiation therapy.
Still, all of the usual treatment options may not always be available to people with breast cancer during the pandemic. In the spring, for example, people may have had to wait weeks or months for certain breast cancer surgeries unless they were diagnosed with an aggressive type of breast cancer. Also, breast imaging was only available for urgent cases, access to new treatments through clinical trials was limited, and fertility-preserving procedures were not available in some places.
Donna-Marie Manasseh, M.D., chief of the division of breast surgery and director of the breast cancer program at Maimonides Medical Center in Brooklyn, NY, said the changes to treatment plans have been stressful for both patients and healthcare providers. But she wants people with breast cancer to know that healthcare providers are carefully considering their decisions, with the goal of providing the best care possible in these circumstances.
“It’s not that the COVID-19 patients became more important than the breast cancer patients,” she said. “We’re making a true, conscious effort to figure out the right things to do for our breast cancer patients — which includes protecting them from COVID-19 and treating their cancer.” In May, when some areas of the country were seeing a drop in COVID-19 cases, the CDC and other health authorities said that healthcare systems should consider providing elective care again. Surgeries, screenings, and other care that had been put on hold started up again in many parts of the United States during May and June. But by late June and early July, restrictions on elective care started again in new hot spots such as Arizona, Texas, and Florida. As the situation evolves, changes in breast cancer care continue to happen in some places.
From www.breastcancer.org
Understanding Deep Vein Thrombosis (DVT) & Pulmonary Embolism (PE)
Dr. Jenice Baker, MD, ER Physician
What are DVT and PE, and how are they related?
DVT is a blood clot in a deep vein, usually in the leg, thigh, or pelvis and can also occur in the arm.
A PE is a blood clot in the lungs and is the most serious condition that can be caused by DVT. This happens when a DVT clot, or part of it, breaks off and travels through the bloodstream to the lungs, reducing or cutting off blood supply. This can be deadly.
HOW MANY PEOPLE ARE AFFECTED BY DVT AND PE?
- According to the CDC, DVT/PE affects as many as 900,000 Americans each year
- PE can cause sudden death in about 25% of cases
Each year, as many as 900k Americans can be affected by DVT/PE
CDC website; data from 2010
WHAT ARE SOME SYMPTOMS OF DVT/PE?
Symptoms of DVT can include:
- Pain
- Swelling
- Tenderness
- Redness of the skin
Symptoms of PE can include:
- Difficulty breathing
- Chest pain or discomfort
- Faster than normal or irregular heartbeat
- Coughing up blood
- Low blood pressure, light-headedness, or fainting
When it comes to these symptoms, this is no time to wait.
Seeking medical attention early may help reduce the chances of DVT or PE becoming more serious. If you experience any of these symptoms, talk to your doctor right away by phone, online, or in person.
Symptoms can also be associated with other potentially serious conditions not related to DVT/PE.
Only a healthcare provider can determine whether these symptoms indicate DVT/PE or another condition.
I had shortness of breath for over a week and finally called my doctor who told me to go to the emergency room. I was admitted with blood clots in my lungs which sounded less serious that pulmonary embolism but is exactly the same thing!! I stopped taking Tamoxifin and started taking blood thinners for 6 months. Now I am fine.
A new study adds to existing evidence linking physical activity with longer survival in women diagnosed with high-risk breast cancer.
Women who engaged in regular physical activity before their cancer diagnosis and after treatment were less likely to have their cancer come back (recur) or to die compared with those who were inactive, the study found.
The study was unusual in that it collected information on the physical activity levels of women with high-risk breast cancer (cancer that is likely to recur or spread) at multiple time points—shortly before their diagnosis, during chemotherapy, and after completion of treatment.
“Our data strongly suggest that the more consistently active patients were, the better they did,” said lead study author Rikki Cannioto, Ph.D., Ed.D., of Roswell Park Comprehensive Cancer Center in Buffalo, NY.
And while survival was extended in women who consistently met federal Physical Activity Guidelines for Americans over time compared with those who did not meet the guidelines, “there was still a survival advantage for women who [were active but] didn’t quite meet the guidelines,” Dr. Cannioto said.
These results “provide evidence that physical activity at any point in time appears to be beneficial for breast cancer survivors,” said Joanne Elena, Ph.D., M.P.H., of the Epidemiology and Genomics Research Program in NCI’s Division of Cancer Control and Population Sciences (DCCPS), who was not involved with the study.
“This study gives us further evidence that being more physically active after a diagnosis of breast cancer is one of the ways that breast cancer survivors can take matters into their hands and improve their health and decrease their likelihood of dying,” said Kathryn Schmitz, Ph.D., M.P.H., an exercise oncology researcher at the Penn State College of Medicine, who also was not involved with the study.
The new study was published April 2 in the Journal of the National Cancer Institute.
Looking at Exercise Over Time
The findings come from the NCI-funded Diet, Exercise, Lifestyle, and Cancer Prognosis (DELCaP) study, led by Christine Ambrosone, Ph.D., also of Roswell Park. The study was embedded in a large clinical trial, led by the NCI-funded SWOG Cancer Research Network, that compared different chemotherapy regimens for women with high-risk breast cancer.
The physical activity analysis by Dr. Cannioto and her colleagues included 1,340 patients from the SWOG trial who also enrolled in the DELCaP study. Participants completed questionnaires about the type, frequency, and duration of recreational physical activity they engaged in at four time points: during the month before diagnosis, during treatment, and at 1 and 2 years after study enrollment. Participants were followed for up to 15 years or until death, with a mean follow-up time of 89 months (7.4 years).
Much, though not all, previous epidemiologic research describing the link between physical activity and cancer outcomes is based on physical activity data collected at only one time point, Dr. Cannioto said.
Using the questionnaire responses, the researchers determined whether participants had met the minimum 2018 Physical Activity Guidelines for Americans at each time point. The guidelines recommend that adults engage in at least 2.5 to 5 hours of moderate-intensity physical activity or 1.25 to 2.5 hours of vigorous-intensity aerobic physical activity per week.
Women with breast cancer who met the minimum physical activity guidelines both before diagnosis and at the 2-year follow-up (after treatment) had a 55% reduced chance of their cancer returning and a 68% reduced chance of death from any cause (not just breast cancer) compared with those who did not meet the guidelines at both times.
Among patients who did not meet the guidelines before diagnosis but met them at the 2-year follow-up, the chance of recurrence or death was reduced by 46% and 43%, respectively, compared with those who did not meet the guidelines at both times. The finding, Dr. Elena said, suggests that “it’s never too late to start exercising to derive benefits.”
The researchers also performed “time-dependent analyses,” which help to account for the fact that physical activity data was collected over multiple time points,” Dr. Cannioto explained.
These analyses showed that, compared with inactive patients, the likelihood of death from any cause was reduced the most among highly active patients, but even patients who regularly engaged in low levels of physical activity saw a substantial survival benefit.
These findings “are good news for breast cancer patients, who can be overwhelmed by the physical activity guidelines, especially during treatment,” when they may be severely fatigued or in pain, Dr. Cannioto said. However, she emphasized, to achieve optimal health benefits, patients and survivors should still strive to meet the guidelines when they are able.
Move as Often as You Can, Whenever You Can
“This study comes at a time when we already have national and international physical activity recommendations for cancer survivors, for the purpose of reducing the risk of recurrence and mortality,” Dr. Schmitz said, and the new findings reinforce these recommendations.
It’s important to keep in mind, however, that “physical activity is not the only factor that determines whether breast cancer will recur, and it certainly is not the only determinant of death. It’s just one piece of the puzzle,” Dr. Elena said.
“We don’t want someone to think, ‘If I exercise enough, I won’t have a recurrence,’” she continued. “But if you can add physical activity into your day, it is likely to influence many types of health outcomes for breast cancer survivors.” That includes quality of life, anxiety, fatigue, and the ability to tolerate treatment, as well as the risk of dying.
The bottom-line message for breast cancer survivors, Dr. Elena concluded, is “Move as often as you can, when you can.”
8 years ago this month at my annual mammogram, I was told I need a biopsy. I had breast cancer. I searched for a surgeon and luckily found Dr. Dahlia Sataloff at Pennsylvania Hospital. She helped me put together a fabulous team- Dr. David Metzer, oncologist also at Pennsylvania Hospital, and Dr. Marissa Weiss, oncologist for my radiation at Lankenau Hospital.
Every year in May (my birthday month), I return to Jefferson Imaging Center to have my annual mammogram and every year I am a wreck before and relieved after (so far). Will I ever think I am totally cured and not worry about it returning??
As nerve wracking as it is, annual mammograms save lives. Catching cancer early leads to a better result. If you haven’t had one and are due, please make your appointment.
The situation in the Imaging Center is coronavirus careful: no magazines, masks on everyone, lots of hand sanitizers all over, no locker, a plastic bag for you clothing, no coffee machine, chairs are 6 feet away from each other.
Stay healthy!!
- Avoid large social gatherings and close contact with people who are sick
- Avoid unnecessary person-to-person contact, such as handshakes
- Avoid touching your eyes, nose, and mouth
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; after blowing your nose, coughing, or sneezing; and before and after coming in contact with others
- Get a flu vaccine
CDC recommends additional additional actions to help keep people at high risk from developing serious complications from COVID-19 healthy in the event of a COVID-19 outbreak in your community, including:
- Stay home as much as possible
- Make sure you have access to several weeks of medication and supplies in case you need to stay home for prolonged periods of time
- When you do go out in public, avoid crowds
- Avoid cruise ship travel and nonessential air travel
- Call 1-800-4-CANCER (1-800-422-6237) Monday through Friday from 9:00 a.m. to 9:00 p.m. ET in English or Spanish. After business hours, recorded information is available.
- Online LiveHelp® chat offers online assistance in English and Spanish Monday through Friday from 9:00 a.m. to 9:00 p.m. ET.
Be sure to get your annual mammogram!!
Here is new information about Breast Cancer and Exercise
Exercise and breast cancer
Regular exercise is an important part of being as healthy as you can be. More and more research is showing that exercise can reduce the risk of breast cancer coming back (recurrence) if you’ve been diagnosed, as well as the risk of developing breast cancer if you’ve never been diagnosed.
A number of organizations, including the American Cancer Society and the American College of Sports Medicine, have published exercise recommendations for people living with and beyond cancer. Still, most people who have been diagnosed with cancer don’t do regular exercise.
There are three basic types of exercise:
- Aerobic exercise uses the large muscles in your body in rhythmic, repetitive motions; examples are walking, running, bike riding, and dancing.
- Flexibility exercise is basically stretching your muscles to keep them elastic and to keep your joints moving freely; examples are yoga, Tai Chi, foam rolling, and stretching.
- Resistance exercise makes your muscles work harder by adding weight or resistance to the movement; examples are weight lifting, resistance band exercises, pull-ups, and push-ups.
New exercise guidelines for people with cancer
An international group of experts reviewed research on exercise for people living with and beyond cancer and developed new guidelines. The new guidelines include specific exercise recommendations to ease common cancer treatment side effects. The experts noted that supervised exercise programs — programs that are led by a trainer or instructor — seem to offer more benefits than unsupervised programs or programs that are done at home.
These new guidelines are different from guidelines released in 2010 that advised cancer survivors to meet the general public health exercise guidelines for all people: 150 minutes of exercise per week.
“With more than 43 million cancer survivors worldwide, we have a growing need to address the unique health issues facing people living with and beyond cancer and better understand how exercise may help prevent and control cancer,” said Kathryn Schmitz, professor of public health sciences at the Penn State College of Medicine and member of the Breastcancer.org Professional Advisory Board, in a statement. Schmitz is one of the authors of the new recommendations.
Overall, the new guidelines recommend people who have been treated for cancer should “avoid inactivity.” To ease the most common cancer treatment side effects and improve health, the experts recommend:
- moderate-intensity aerobic exercise at least 3 times per week, for at least 30 minutes
- resistance exercise at least 2 times per week, doing at least 2 sets of 8 to 15 repetitions, using a weight or resistance that is at least 60% of a person’s one-repetition maximum
Exercise recommendations to ease specific side effects are:
- Anxiety: 30-60 minutes of moderate-intensity aerobic exercise 3 times per week for 12 weeks, or twice weekly combined 20-40 minutes of aerobic exercise plus 2 sets of 8-12 repetitions of resistance exercise for 6 to 12 weeks.
- Depression: 30-60 minutes of moderate-intensity aerobic exercise 3 times per week for at least 12 weeks, or twice weekly combined 20-40 minutes of aerobic exercise plus 2 sets of 8-12 repetitions of resistance exercise for 6 to 12 weeks.
- Fatigue: 30 minutes of moderate-intensity aerobic exercise 3 times per week.
- Quality of life: Combined 30 minutes of moderate-intensity aerobic exercise plus 2 sets of 12-15 repetitions of resistance exercise 2 to 3 times per week for at least 12 weeks.
- Lymphedema: A supervised resistance exercise program that slowly ramps up the resistance and focuses on the large muscle groups 2 to 3 times per week can help people with upper extremity lymphedema related to breast cancer treatment. For many years, doctors recommended that women skip exercise to reduce the risk of lymphedema or avoid making the condition worse. But more recent research has shown that a careful exercise program, supervised by a professional with knowledge about lymphedema, that starts low and increases slowly, can offer benefits. The researchers noted that the lymphedema exercise prescription was designed for safety or no harm rather than preventing lymphedema symptoms. The experts also noted that there isn’t enough evidence to decide if starting a resistance training program without supervision is safe for women with lymphedema or at-risk for the condition.
- Physical function: 30-60 minutes of moderate-intensity aerobic exercise, 2 sets of 8-12 repetitions of resistance exercise, or combined 20-40 minutes of aerobic exercise plus 2 sets of 8-12 repetitions of resistance exercise 3 times per week for 8 to 12 weeks.
“Through our research, we’ve reached a point where we can give specific FITT exercise prescriptions — which means frequency, intensity, time, and type — for specific outcomes like quality of life, fatigue, pain, and others,” Schmitz said. “For example, if we’re seeing a head and neck cancer patient with a specific set of symptoms, we could give them an exercise prescription personalized to them.
“Currently, an average person on the street will know that exercise is good for preventing and treating heart disease, but not for melanoma,” she added. “We want to change that. When researchers in the 1950s built an evidence base for exercise and heart disease, there was a shift in public knowledge about that connection. It’s now time for the same thing to happen with exercise and cancer.”
Exercise safely
Because being diagnosed and treated for cancer can change how people move and function, the experts recommended that people tell their doctors they plan to start an exercise program and ask if they have any health conditions that may limit what they can do.
The researchers also recommended that people have a thorough evaluation of all aspects of their physical fitness before starting an exercise program, including strength, endurance, body composition, and flexibility.
Still, the experts did not want a doctor’s approval or a fitness evaluation to be a barrier to people exercising. If either one of these items is difficult to get, the experts recommended that a person start a low-intensity aerobic program, such as walking or slow bike-riding, or gentle stretching, with a slow increase in intensity.
What this means for you
If you’re recovering from breast cancer treatment, along with being busy with work, household chores, and family matters, finding time to exercise almost every day can seem impossible.
Still, these new recommendations allow you to break up your exercise into 20- or 30-minute sessions 2 to 3 times per week, rather than trying to find the time and energy to work out for an hour or more at one time.
Walking can be a great way to start. Maybe you walk 30 minutes before going to work and 20 minutes on your lunch break. You can add a few more minutes by parking farther away from your building or taking mass transit. Or you can make plans to walk with a friend after work — you’re more likely to stick with an exercise plan if someone else is counting on you. Plus, you can socialize at the same time.
Along with healthy diet and lifestyle choices, regular exercise is one of the best things anyone who has been diagnosed with breast cancer can do to feel their best and to keep the risk of breast cancer recurrence as low as it can be. This study adds to other research suggesting that regular exercise can help keep your physical and mental health in top shape. No matter how old you are, it’s never too late or too soon to get moving. And once you do start, keep at it!
Visit the Breastcancer.org Exercise section for tips on exercising safely and how to stick to an exercise routine.
To talk with others about the benefits of exercise, share exercise tips, and get encouragement, join the Breastcancer.org Discussion Board forum on Fitness and Getting Back in Shape.
Written by: Jamie DePolo, senior editor
From www.breastcancer.org
Happy day!! I got my annual mammogram at Jefferson- Honickman Breast Imaging Center and all is well- 7 years post-breast cancer!!! Annual mammograms helped them find it small and very fixable!!
Please schedule your annual mammogram! I have my appointment for 2020.
Each year on May 8th, women living with ovarian cancer, their families and supporters, along with patient advocacy organizations from around the world, come together to raise awareness about ovarian cancer. World Ovarian Cancer Day (WOCD) is the one day of the year we all raise our voices in solidarity across the world in the fight against this disease.
The first World Ovarian Cancer Day took place in 2013. World Ovarian Cancer Day is an initiative of the World Ovarian Cancer Coalition.
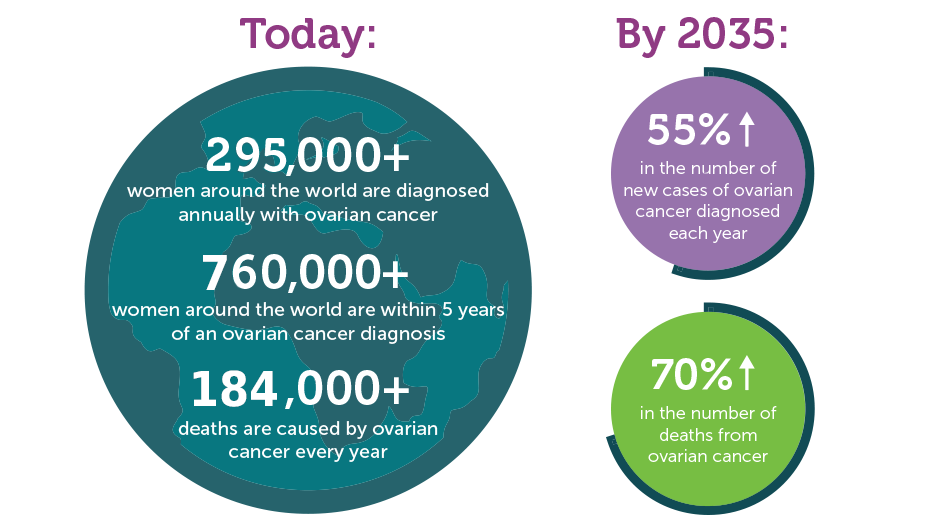
Why do we need World Ovarian Cancer Day?
Ovarian cancer has the lowest survival rate of all female cancers. Most women are diagnosed once the cancer has already spread, making it more difficult to treat. There are often delays in diagnosing ovarian cancer. That is because there is no early detection test, and symptoms are often confused with symptoms of other less severe illnesses, particularly gastrointestinal complaints.
Five-year ovarian cancer survival rates vary around the world, ranging from 30% to 45%. By comparison, five-year survival rates for women with breast cancer range from 80% to 90%.
Ovarian cancer is overlooked and underfunded – yet every woman in the world is at risk of developing this disease.
That is why we need World Ovarian Cancer Day!
World Ovarian Cancer Day makes a difference
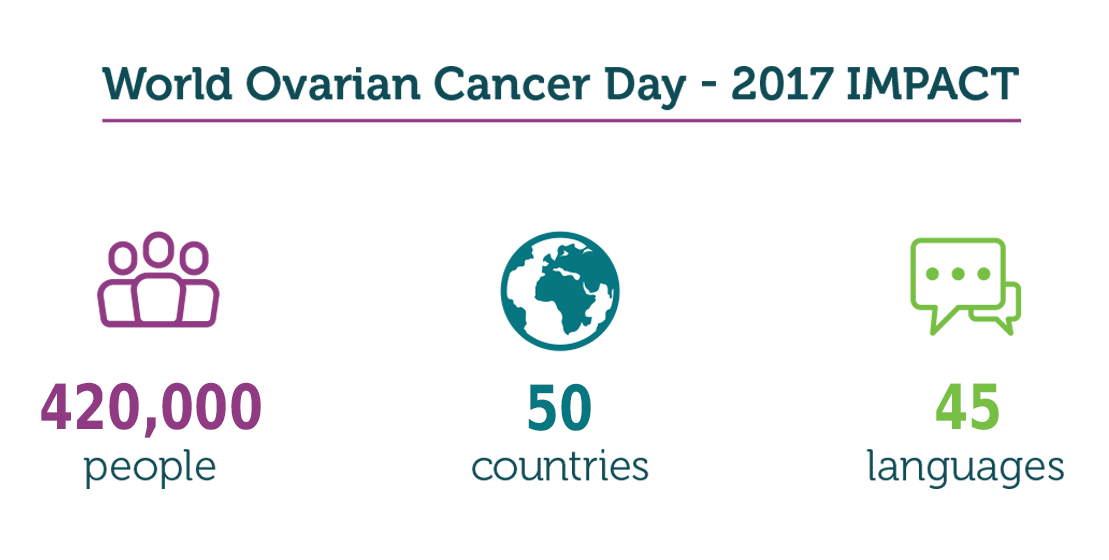
The impact of World Ovarian Cancer Day continues to increase! In 2018, the World Ovarian Cancer Day awareness campaign reached over 420,000 people, with supporters from 50 different countries and 45 different languages taking part.
Every time the World Ovarian Cancer Day awareness messages are shared – every Tweet, retweet, Facebook post, Like and Share – you are helping to spread the ovarian cancer message around the world. Your voice has power.
How chronic stress boosts cancer cell growth

Researchers now know how chronic stress fuels the growth of cancer.
Chronic stress, which a person has consistently over a long period of time, affects mental and emotional well-being as well as physical health.
Studies have tied chronic stress to accelerated cognitive impairment, a higher risk of heart problems, and problems with gut health.
Previous research also suggests that exposure to stress could speed up the growth of cancer through its impact on gene activity.
Now, researchers from the Dalian Medical University in China — in collaboration with colleagues from across the world — have located a key mechanism, which chronic stress triggers, that fuels the growth of cancer stem cells that tumors originate from.
More specifically, the researchers have studied this mechanism in mouse models of breast cancer.
Their findings — which they report in The Journal of Clinical Investigation — point the finger at the hormone epinephrine, but they also suggest a strategy to counteract the effects of stress mechanisms on cancer cells.
“You can kill all the cells you want in a tumor,” notes co-author Keith Kelley, from the University of Illinois at Chicago, “but if the stem cells, or mother cells, are not killed, then the tumor is going to grow and metastasize.”
“This,” he adds, “is one of the first studies to link chronic stress specifically with the growth of breast cancer stem cells.”
Stress fuels tumor growth
To see how stress would impact cancer cell growth in the rodents, the researchers put all the mice in small, restrictive enclosures for a week. Then, they split the mice into two groups.
They put one group into large, comfortable enclosures to discontinue the stress; these mice acted as the control group. The other group stayed in the small enclosures for another 30 days; these mice acted as the experimental group.
Following their initial investigation, the scientists saw not only that the stressed mice exhibited changes in behavior that were indicative of depression and anxiety, but also that they had larger cancer tumors than their peers in the control group.
Also, these tumors were growing at a faster rate, and on the whole, the stressed mice also had a greater number of cancer stem cells than the other mice. Still, at this point, it remained unclear exactly how stress contributed to the progression of cancer.
According to principal investigator Quentin Liu, from the Institute of Cancer Stem Cell at Dalian Medical University, “The direct signaling network between stress pathways and a cancer-propagating system remains almost completely unknown.”
He adds, “A better understanding of the biochemistry that causes stress to increase the growth of cancer cells could lead us toward targeted drug interventions, one of which we discovered in this work.”
Blame epinephrine, not cortisol
When they looked into how various physiological factors changed in the mice that had experienced chronic stress, the researchers closed in on a hormone called epinephrine.
The stressed mice had much higher levels of this hormone than the mice in the control group. Also, in mice from the experimental group that had received a drug that blocked ADRB2 — which is an epinephrine receptor — cancer tumors were smaller and the numbers of cancer stem cells were also lower.
“When most people think of stress,” says Kelley, “they think it’s cortisol that’s suppressing the immune system.” However, he adds, “The amazing thing is cortisol was actually lower after a month of stress.”
How does epinephrine help cancer stem cells thrive? The authors explain that when this hormone binds to ADRB2, the interaction boosts levels of lactate dehydrogenase, an enzyme that normally gives muscles an “injection” of energy in a danger situation. This allows the person to either fight the threat or run away from it.
A byproduct of this energy boost is the production of an organic compound called lactate. In the case of people with cancer, the harmful cells actually feed on this compound; it allows them to acquire more energy.
This means that if a person has chronic stress, they will have too much lactate dehydrogenase in their system. This, in turn, will activate genes related to cancer growth and allow cancer cells to thrive.
“These data provide a novel pathway that explains how elevated epinephrine caused by chronic stress promotes breast cancer progression by acting directly on cancer stem cells.”
Quentin Liu
Is vitamin C the answer?
Next, the researchers validated their results by studying blood epinephrine levels in 83 people with breast cancer.
Sure enough, they found that people with high blood levels of epinephrine also had excess lactate dehydrogenase in cancer tumors — which the researchers had access to through breast cancer biopsy samples.
Also, people who had higher levels of the stress hormone were likelier to have poorer outcomes following treatment when compared with people with lower epinephrine levels.
Next, the scientists tried to see whether or not they could identify a strategy to block epinephrine’s ill effects on the system. In laboratory tests on breast cancer cell lines, they analyzed the effects of a few Food and Drug Administration (FDA)-approved drugs on lactate dehydrogenase production.
The most promising substance that the investigators settled on was actually vitamin C, which blocked actate dehydrogenase production in laboratory experiments. When the investigators tested this approach in mouse models, they obtained the same results: Stressed mice they’d injected with vitamin C experienced tumor shrinkage.
“Taken together, these findings show that vitamin C might be a novel and effective therapeutic agent for targeting cancer in patients undergoing chronic stress,” concludes Liu.



